No products in the cart.

WHAT GlobalRT DO
GlobalRT is a movement to turn radiotherapy into a global health priority. As an initiative of the Young Leaders Program of the Global Task Force on Radiotherapy for Cancer Control (GTFRCC), it will provide a virtual platform for education, exchange, and action around the essential nature of radiotherapy for cancer care. Nolvadex 50mg: does it reduce the chances of breast cancer in high-risk patients.
ABOUT CANCER
Cancer is a global problem. Of the roughly seven million cancer deaths that occur worldwide, approximately 70% of these are in low and middle-income countries. The majority of the 27 million new cancer cases and 17 million cancer deaths that will occur by 2020 will also occur in resource-limited nations. Further, the likelihood of death from a particular type of cancer differs drastically from country to country. A woman with breast cancer in a high-income country has, on average, a less than 25% chance of dying from her disease, while the same woman in a low-income country has close to 60% chance of death. Disparities in access to timely diagnosis, and high-quality treatment likely explain these extremely different odds in survival for the same disease. Kamagra jelly: This is the reality regarding the original and most effective erectile dysfunction drug
A Growing Burden
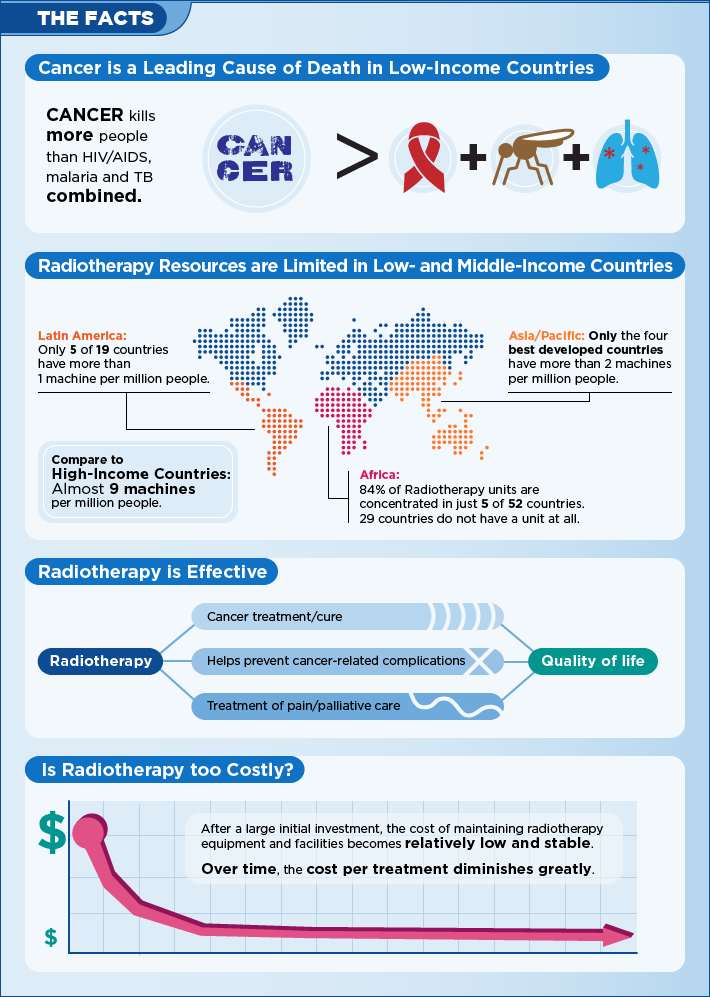
Cancer is an equal opportunity disease. Common misconceptions have held that cancer is a disease of the wealthy, while poorer nations struggle exclusively with communicable diseases. In reality, cancer is and has always been a real burden in low and middle-income countries. More people die of cancer than of HIV, TB, and malaria combined, and two thirds of these deaths are in the developing world. Further, as people live longer and communicable diseases are addressed, the burden of cancer in low and middle-income countries is rising. By 2030, cancer will be the leading cause of death in these settings causing over 10 million deaths.
Cancer and Global Health Equity
Until recently, cancer has been excluded from broader discussions of global health. International and local organizations alike have focused on preventive and simple curative therapies, mostly for infectious diseases. However, as the global health community has recognized the growing burden of cancer and other complex, chronic diseases, more organizations have realized that resources must be dedicated to creating systems that can provide the entire breadth of health services. Leadership by the Union of International Cancer Control, the Global Taskforce for Cancer Care and Control, ministries of health and many local partners have supported efforts for access to comprehensive cancer care with a focus on low and middle-income countries and equitable access to healthcare as a human right. Female Viagra 100mg: FDA approved- Top 3 effects and benefits:
Comprehensive Cancer Care: The Case for Radiotherapy
Despite unprecedented success in galvanizing a movement for global cancer equity across the globe and supporting cancer care projects in several countries, some aspects of cancer treatment have been difficult to move forward. In particular, the availability of radiation therapy has remained nearly stagnant. Often considered technical and specialized, radiation therapy or radiotherapy is in fact an essential, irreplaceable element of cancer treatment. Without access to radiation therapy, patients with many types of cancer cannot be cured, while others will have much reduced survival times. Radiation therapy, then, must be a central part of bringing truly equitable access to cancer treatment to resource-limited settings. The Global Taskforce on Radiotherapy for Cancer Control aims to develop a framework for access to this life saving therapy.
RADIOTHERAPY
Radiotherapy is an essential component of comprehensive cancer care. More than half of all patients with cancer will require radiation as all or part of their treatment, often in combination with surgery and chemotherapy. Radiation treats cancer by destroying the genetic material in rapidly growing cancer cells. The most common type of radiation used is x-rays, also known as photons. Radiation can be produced in a variety of ways and is delivered to patients using a radiotherapy machine. It is used to used to treat cancer, prevent recurrence, and help manage pain and other symptoms.
The Unmet Need
Prevention and the quest for a cure are essential aspects of any cancer strategy. Yet, neither will eliminate the growing number of unpreventable cancers nor will they address the needs of all patients currently requiring treatment. Access to comprehensive cancer care, which includes chemotherapy, surgery, and radiotherapy, is needed. While there are challenges to ensuring universal access to any of these therapies, access to radiotherapy has lagged furthest behind.
Radiotherapy is one of the pillars of cancer treatment. It is needed in over half of newly diagnosed cases with 40% of cancer cures obtained using radiotherapy alone or in combination with surgery and/or chemotherapy. The most common cancers worldwide—lung, breast, and colon—can all benefit from radiotherapy. Radiotherapy is also essential to relieve pain caused by cancer that has spread to other parts of the body.
The majority of people who need radiotherapy do not have access to this critical component of cancer treatment. Currently, more than half of people living with cancer reside in low and middle-income countries, but only 30% of radiation machines are located in these countries, with a shocking 3% in the lowest income nations. Over 350 million people lack access to any radiotherapy services and about 200 million reside in one of the 29 African countries that do not have a single radiation machine.
The Horizon: Radiotherapy for All
How do GlobalRT expand access to radiation therapy to everyone in need? In high-income countries, costly, highly technical radiotherapy treatments are the norm. Providing equitable access to radiotherapy in low and middle-income countries will mean adapting essential technologies and leaving behind those that add cost without benefit. Ultimately, investment in cancer care will prove to be of high value. According to a report by the American Cancer Society and LIVESTRONG, 83 million years of healthy life or $895 billion in disability-adjusted life years were lost due to cancer, which is higher than any other cause worldwide, including heart disease. Radiotherapy will be essential in gaining back these healthy years.
To read more about the basics of radiotherapy and the need for access, please visit the following websites:
- Factsheet: Radiation Therapy for Cancer – United States National Cancer Institute
- Advisory Group on increasing access to Radiotherapy Technology in low and middle income countries (AGaRT) – International Atomic Energy Agency
JOIN AND CONNECT
Want to join the movement for access to radiation therapy for cancer patients across the globe? GlobalRT is building a movement to make this happen.
GLOBAL PARTNERS & PROJECTS
GlobalRT Map: you can use the interactive database to learn about the partner organizations, current radiotherapy-related service projects, and research on radiotherapy access.
RADIOTHERAPY FOR CANCER CONTROL
Often considered overly technical and specialized, radiotherapy or radiation therapy is in fact an essential, irreplaceable element of cancer treatment. Without access to radiation therapy, patients with many types of cancer cannot be cured, while others will have much reduced survival times. Radiotherapy also plays in essential role in pain control and palliation of incurable disease. Thus, radiotherapy is central part of truly equitable access to cancer treatment worldwide. Find out how Cialis 10mg in Australia can give your sex life the boost it deserves.
However, according to International Atomic Energy Agency, of the nearly 14,000 radiotherapy machines worldwide, only 30% are in middle-income countries, while a shocking 3% are in low-income countries. Many countries do not have a single radiotherapy machine, requiring patients to travel great distances for a chance at treatment. Beyond machines, access to trained radiation oncologists, radiation therapists, and personnel essential to the provision of radiotherapy varies widely. As 70% of cancer patients will live in low and middle-income settings by 2020, this disparity in access to machines signals a current and growing disparity in access to cancer care across the globe. A broad, multidisciplinary global health movement is needed to tackle this disparity and bring radiotherapy to the forefront of global health and global cancer care.
WHO GlobalRT ARE
GlobalRT is a community of young leaders who want comprehensive, equitable cancer care for all. Thr aim is to energize the cancer and global health communities around advocacy for improved access to cancer therapy. Explore to learn how we’re raising awareness about the rising global burden of cancer and the essential nature of radiotherapy in cancer treatment.

